GPT-5 Just Outscored Your Doctor on Medical Exams
The latest AI model crushed human physicians on licensing tests, but real-world medicine isn't multiple choice
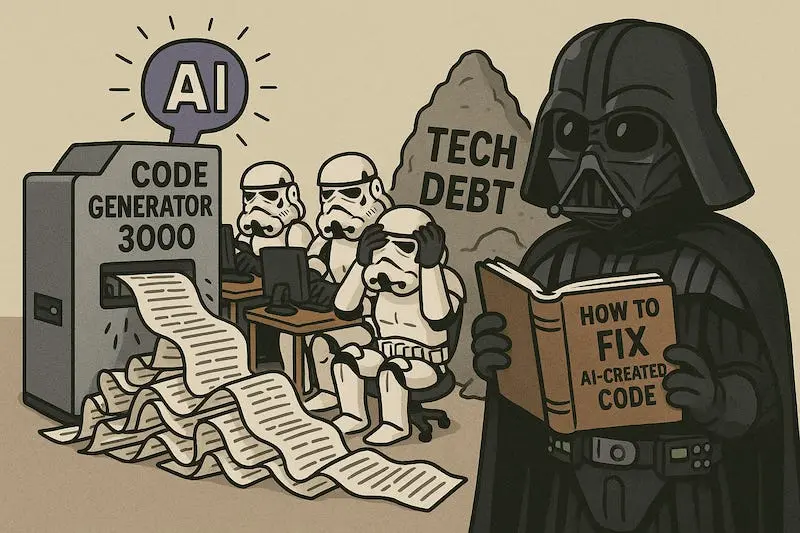
When the Test Becomes the Target
GPT-5 just aced the US medical licensing exam with scores that would make any medical student jealous. The model achieved “state-of-the-art accuracy across all QA benchmarks” according to the alphaXiv study ↗, outperforming pre-licensed human experts by nearly 30% in reasoning and understanding tasks. On multimodal medical reasoning tasks, where the AI processes both text and images, GPT-5 delivered a staggering 29% improvement over its predecessor GPT-4o.
The numbers look impressive until you realize what they’re measuring: pattern recognition on standardized tests, not clinical competence. As one observer noted, “One human is not as good as a computer with a built-in library of knowledge that took centuries to digest and understand.” True, but that computer also can’t feel a patient’s abdomen or notice the subtle tremor in their voice.
The Benchmark Blind Spot
Medical licensing exams follow predictable patterns. They test established knowledge, diagnostic algorithms, and textbook scenarios. GPT-5 excels at these structured challenges because it’s been trained on mountains of medical literature, guidelines, and case studies. The model can recite drug interactions, diagnostic criteria, and treatment protocols with near-perfect recall.
But real medicine happens in the messy gaps between multiple-choice options. It’s the 2 AM emergency room decision when the patient’s symptoms don’t match any textbook description. It’s recognizing when a “non-compliant” patient is actually struggling with transportation to the pharmacy. These nuances escape even the most sophisticated AI when it’s measured against clean, curated test data.
When the Questions Get Weird
The cracks appear when researchers slightly alter the test conditions. A separate JAMA Network Open study ↗ found that frontier AI models “fail spectacularly when the familiar formats of medical exams are even slightly altered.” When researchers replaced correct answers with “none of the other answers”, GPT-4o’s accuracy dropped by 25%. Meta’s Llama model showed a nearly 40% decline.
This isn’t just academic, it reveals how these systems actually work. They’re pattern matchers, not reasoners. As Stanford researcher Suhana Bedi explained, “It’s like having a student who aces practice tests but fails when the questions are worded differently.” The models struggle with administrative and clinical decision support tasks that require actual reasoning rather than pattern recognition.
The Real-World Consequences
Hospitals are already deploying AI for administrative tasks and preliminary diagnostics, but the licensing exam results create dangerous expectations. When Google’s former AI lead suggests ↗ skipping medical school because AI will obsolete doctors, he’s missing the fundamental point: clinical medicine requires human judgment, not just information retrieval.
The most telling finding from the research isn’t GPT-5’s test scores, it’s the disclaimer that “until these systems maintain performance with novel scenarios, clinical applications should be limited to nonautonomous supportive roles with human oversight Translation: great assistant, terrible physician.
The medical profession isn’t facing obsolescence, it’s gaining powerful new tools. But the tools only work when wielded by skilled human hands that understand their limitations. GPT-5 might outperform humans on multiple-choice exams, but it still can’t sit with a frightened patient and explain why their treatment plan is the right choice.